Interviews

Regenerating Teeth and Bones With iPS Cells (Part 2)
Hiroshi Egusa
A low-cost, genius solution to combat one of the largest issues with iPS cell regeneration
Interviewer & Japanese Writer: Yamamoto Takaya; Translation & Editing: Matthew Cherry
Dr. Hiroshi Egusa saw his research progress even further thanks to the support he received from the INNO-vation Program. He was working on regenerative bone therapy, specifically how to prevent tumors from forming through the regeneration process.
(Click here to read Part 1)
Since iPS cells are known to take on the properties of other cells, they can be used for regenerating bones. Controlling iPS cells effectively can prove to be difficult and tumor formation is a particularly common issue when using these cells in bone regeneration therapy.
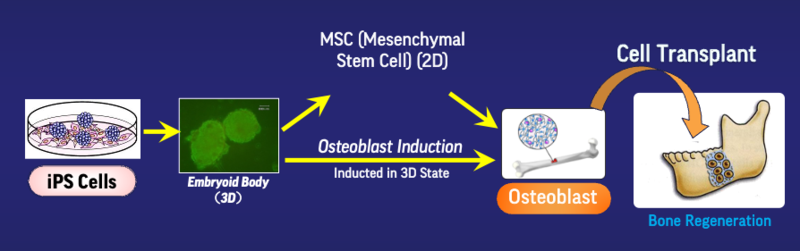
Bone regeneration therapeutic process using iPS cells
Because iPS cells are living cells, they can become uncontrollable, which is a leading cause of tumor formation. “Therefore, I thought if I could inactivate the iPS cells by freeze-drying them, they could be used even if they weren’t in a living state,” Dr. Egusa said.
Simply inactivating the iPS cells turned out to be inadequate for the procedure, as it was still hard to control them well enough to change them into bone cells. By adding gene manipulation into the mix, inactive, freeze-dried iPS cells were shown to regenerate as bone in areas where the bone matter was missing. Egusa said that using this method through animal experimentation led to the discovery of bone regeneration without the formation of tumors.
This freeze-drying approach to inactivating iPS cells (and thus preventing tumor formation) holds tremendous potential. That’s not to say it’s the only benefit of the therapy, however. Once iPS cells are placed in an inactive state, they cease to be recognized as living organisms in the medical field. This makes it easier to obtain approval for their use, as they are treated as medical devices rather than living cells.
It’s also possible that enveloping these inactive, freeze-dried iPS cells with other materials may improve their regenerative effects. Although there is still much to be discovered with the potential in iPS cell-related developments, the research behind it has been progressing tremendously in recent years. But there’s still one aspect that’s keeping this research from progressing into reality.
That would be the cost. Cultivating iPS cells is associated with an extremely high monetary cost. Traditional artificial bone material made by chemically synthesizing apatite with other materials is relatively inexpensive, which makes the conventional method the overwhelmingly superior choice when it comes to controlling costs.
“Regenerated bones using iPS cells are expected to be sturdy and adhere strongly to the patient’s body. But the perceived effectiveness of medical care doesn’t always translate to higher medical value. The common denominator in all medical care is cost. If the cost goes up, the value it presents for medical care goes down. In order to release new forms of medical care into the world, controlling the costs is extremely crucial. How exactly one achieves this is currently a matter of much discussion,” Egusa said about the reality of the situation.
In Part 3, we’ll ask Dr. Egusa about his work after the INNO-vation Program.

Continued in Part 3 (coming November 21st, 2022)
Hiroshi Egusa's Profile

